Update
Antimicrobial Resistance and the Environment
Ranking among the top 10 threats to global health, antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi and parasites change in ways that render ineffective the medications used to cure the infections they cause. Although AMR occurs naturally, it is facilitated by the misuse and overuse of antibiotics in human health, food-animal production and agriculture, alongside environmental factors such as pollution and poor waste management. AMR depends greatly on the interaction between humans, animals and the environment, hence, adopting a One Health approach is critical for developing appropriate responses.
Antimicrobial Resistance (AMR) as a Global Threat
Antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi and parasites change in ways that render ineffective the medications used to cure the infections they cause (WHO, 2017). Antimicrobials-resistant microorganisms can become resistant to plural antibiotics, becoming so-called superbugs. AMR is among the top 10 threats to global health (WHO, 2019). In 2019 alone, AMR was the direct cause of 1.27 million deaths and a complicit cause of 4.9 million deaths, making drug-resistant infections more deadly than HIV/AIDS or Malaria (Lancet, 2022). This figure may drastically increase in future years, with estimated 10 million annual deaths by 2050 due to AMR (UNEP, 2023). AMR also poses economic challenges, leading to at least USD 3.4 trillion annually by 2030 of GDP drop and increasing by 24 million the number of those living in extreme poverty (UNEP, 2023). On top of that, antimicrobials are a powerful ally to cure infections, and the increasing resistance to those without the development of new antimicrobials poses a challenge to human, animal and plant health.
AMR is a natural response that is both intrinsic and genetically acquired. Nevertheless, various factors favor its increase and fuel a dangerous rate of antibiotics ineffectiveness. The main drivers indicated by World Health Organization are:
- the misuse and overuse of antimicrobials;
- lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals;
- poor infection and disease prevention and control in health-care facilities and farms;
- poor access to quality, affordable medicines, vaccines and diagnostics;
- lack of awareness and knowledge;
- and lack of enforcement of legislation.
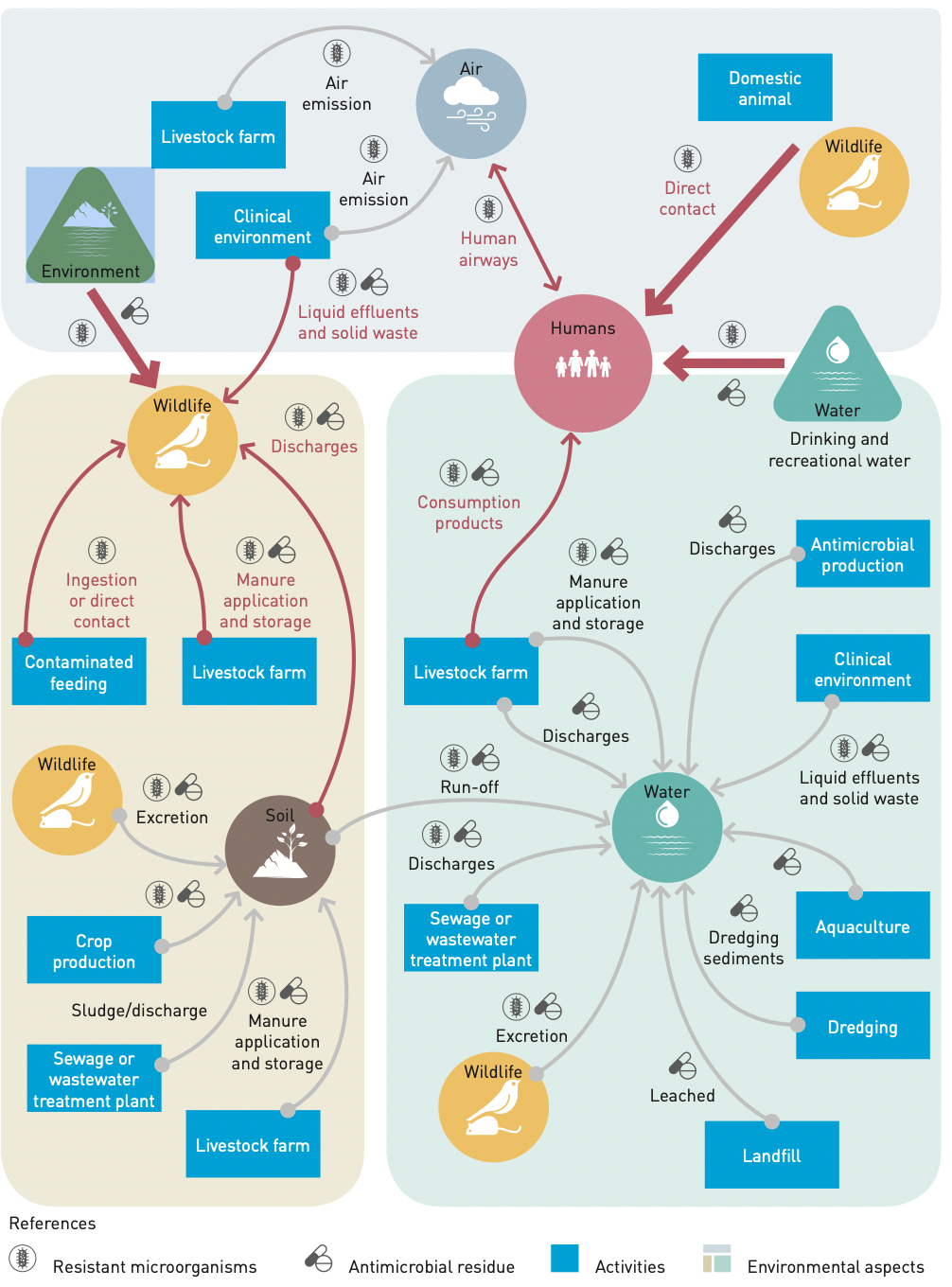
These factors have an important environmental dimension as waterways, air and soil act as means of transmission and increasing temperatures and hazards associated with climate change contribute to greater development and the spread of antimicrobials and consequently increase resistance to their effectiveness.
AMR and the Environment
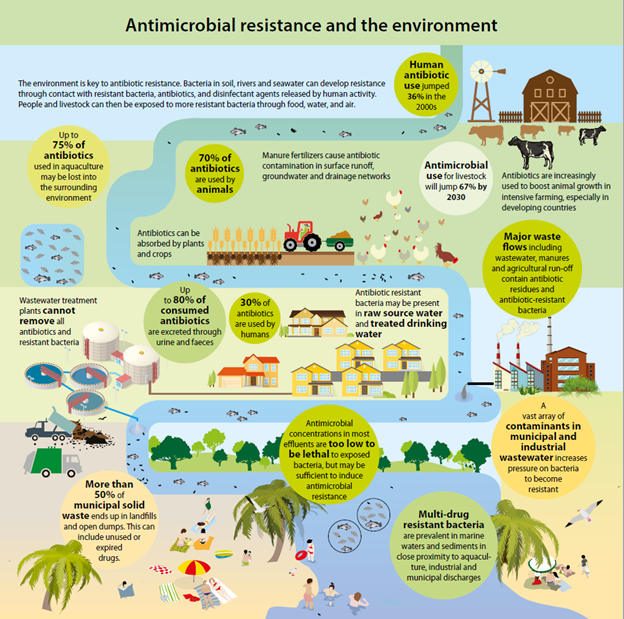
The environment and the AMR pandemic are strictly linked. The environment is both a vehicle for spreading AMR microbes and a culprit of antimicrobial pollutants, which negatively impact biodiversity and ecosystems (UNEP, 2022).
Source: Healthy environment is key for antibiotics to work | UNEP | 2020
The spread of antimicrobials and the consequent increases in antimicrobial resistance occurs especially through unsound release of residues into the environment (UNEP, 2017). Therefore, environmental degradation and pollution factors connected to the triple planetary crisis of climate change, biodiversity loss and pollution are the very same ones that alter microbial diversity and facilitate the development, transmission and diffusion of AMR (UNEP, 2022).
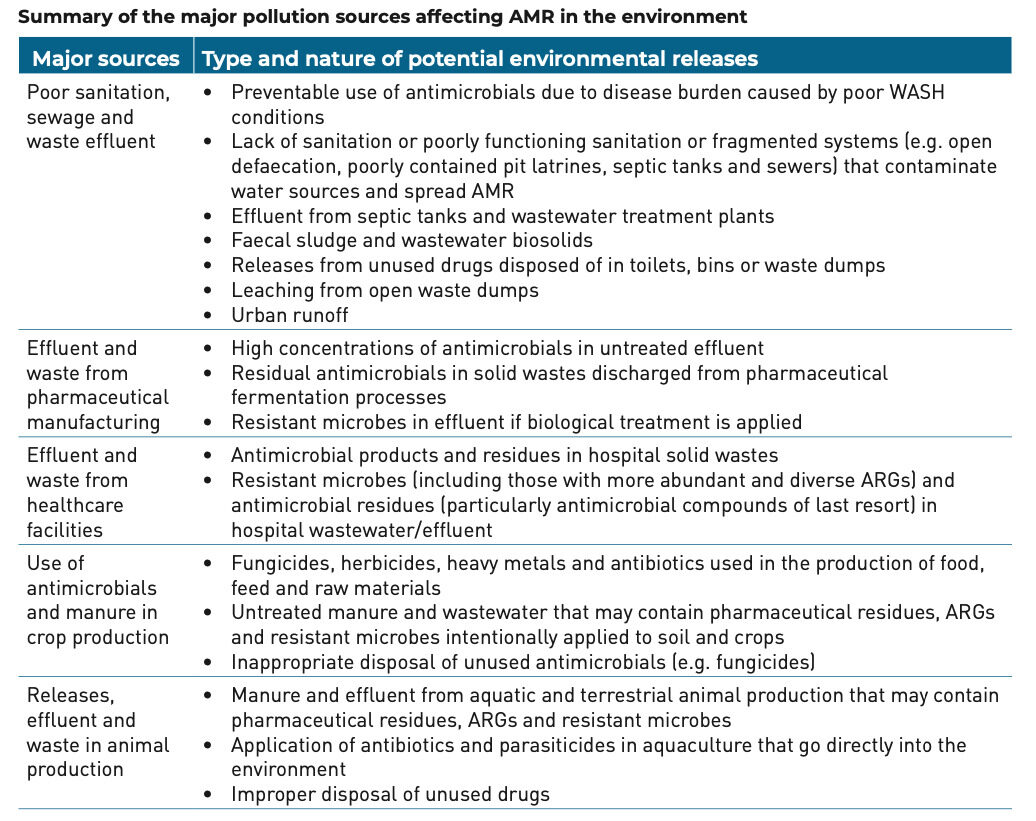
The dumping of these substances in the environment occurs mainly through five pollutant sources.
Source: Environmental Dimensions of Antimicrobial Resistance. Summary for Policymakers | UNEP | 2017.
Antimicrobials coming from these sources are present and transmitted through water (rivers, lakes and sediments), sewage, soil, air and wildlife. They represent a serious threat as their spread is not limited to the specific points where the contamination occurs (transient source), but it spreads in a diffuse and non-source way.
Source: Bracing for Superbugs. Strengthening environmental action in the One Health reponse to antimicrobial resistance | UNEP | 2023
In the past years due to the COVID-19 pandemic, zoonotic diseases have raised attention and preoccupation. As antibiotics are more frequently used in animal husbandry, resistance is rapidly developed and spread through the environment in the shape of unmetabolized antibiotics. The transmission of diseases from animals to humans through zoonotic pathogens bears the risk of communicating also antibiotic resistant genes (ARGs) through contact or consumption of animal products. Therefore, people working in or living close to livestock facilities are disproportionately at risk.
The effects of AMR on the environment
As previously mentioned, the impact of antimicrobial pollutants on AMR in the environment is complex and necessitates further evidence. The pollution of waterways, soils and air are certainly contributing to environmental degradation, as they are to growing levels of antimicrobial resistance.
AMR and the Triple Planetary Crisis
Climate Change
Increased temperatures associated with climate change are an important factor for the development of diseases such as bacteria, viruses, parasites, fungi and vector-borne diseases in humans, animals and plants, which might survive more easily in higher temperatures. This may cause the insurgence of more antimicrobial-resistant diseases. Climate change-related hazardous events like floods that ravage human settlements increase the likelihood and frequency of uncontrolled leakage of antimicrobials into the environment and in communities.
Biodiversity Loss
Healthy soils are home to high microbial diversity, which is key to performing vital ecosystem functions. Antimicrobials have ecotoxicological effects that can disturb soil and plant health, reducing soil microbial diversity. Soil microbial diversity is an essential shield for the spread of AMR, as well as a main source of pharmaceutical discoveries. Soil microbial composition has been altered by human activities and climate change. Further research is necessary to establish how AMR affects biodiversity loss (UNEP, 2023).
Pollution and Waste
Antimicrobials as pollutants to the environment come from multiple sources. The most harmful and threatening ones are treated and untreated human and animal excreta, residual waste from the pharmaceutical, manufacturing and healthcare sectors that leak into the environment through air, soil and waterways.
AMR and Health
Antimicrobial resistance is a global health threat. The improvement in antibiotics availability in the world has resulted in increased consumption, with last-resort treatments being employed more and more frequently. As humans, animals and plants grow resistant to treatments, the risk of developing serious health conditions from even mild infections grows. To contrast the ineffectiveness of current antimicrobials, the demand for new ones is increasing. Nevertheless, for new antimicrobials to not fall ineffective, it is fundamental to change and monitor antimicrobial use (AMU).
AMR also represents a burden for healthcare systems globally as hospitalizations become more frequent while curable with antibiotics. According to WHO, a high incidence of AMR is encountered in the treatments for common infections like urinary tract infections, sepsis, sexually transmitted infections, and some forms of diarrhoea. Healthcare facilities, care homes, pharmacies and prisons also are hotspots for AMR development and spread as the vast array of chemicals and medicines employed can alter the antimicrobial environment. In addition, antimicrobials administered in healthcare facilities easily end-up in their wastewater, making safe and adequate management an imperative to avoid dangerous outbreaks around infrastructures that hosts people in fragile situations.
AMR in Agriculture and Animal Farming
Antibiotics are largely used in animal farming and agriculture to manage diseases, maintain health and favor growth. Animal farming and production contribute to spiking antimicrobial resistance through a self-reinforcing loop. As manure coming from antibiotics-fed animals and run-off contaminated water are used to fertilize and irrigate fields, antibiotics can concentrate in soils. Similarly, as fertilizers like pesticides are directly applied to the environment, animals and humans are more likely to enter into contact with these drugs.
Consumption of animal products has been up-trending in the past years, leading to the intensification and adoption of antibiotics to keep up with the demand. Animal production is linked to AMR in complex ways. On the one hand, animals are given antibiotics that are then contained in foods, increasing the likelihood of foodborne diseases (FAO, 2023). According to FAO, 27 different antimicrobial classes are administered to animals. Some of these are important for human health and considered ‘last resort’ treatments, therefore, exposure to these antibiotics through food bears the risk of raising antimicrobial resistance. Then animals are often fed zinc and copper additives as an additional antimicrobial resource.
An example of food-borne diseases that can be transmitted to humans through food consumption is Salmonella, contained in chicken and pork meat. On the other hand, antibiotics used in animals represent a risk as their manure is often employed to fertilize crop-producing soils, changing the soils’ biota and impacting the products. Similarly, animal agricultural waste is often released in waterways, contaminating waters that are often employed to irrigate fields. Water-borne contamination is also a serious concern in aquaculture. Antimicrobials are released in ponds and tanks where fish is raised, and water is then often released into the environment. Studies are yet to quantify impacts but have already observed changes in the biodiversity around the areas where antimicrobials are used in aquaculture. Currently, the impact of AMR on animal health is yet uncertain and initiatives like the Global Burden of Animal Diseases (GBADs) programme are monitoring it.
The crop production sector has seen exponential growth in the use of pesticides with antimicrobial properties (ex. Fungicides) in the past thirty years (FAO, 2022). Pesticides are especially dangerous for AMR since they are directly applied to the environment resulting in higher concentrations (UNEP, 2023) and depending on their kind and quantity, they can be toxic to human health.
AMR and Pharmaceutical and Chemical Production
The pharmaceutical and chemical production sectors are one of the three main sources of the spread of antimicrobial resistance globally. Antimicrobial spillovers into the environment occur across the whole production value-chain. During the manufacturing and production phases, chemicals, microorganisms and genes contributing to AMR are often released as a result of poor regulations against pollution, and the absence of manufacturing standards to counter AMR. The main place of pollution from pharmaceutical and chemical production industries are surface waters that are contaminated with active pharmaceutical ingredient (API) wastewaters.
International Cooperation on AMR
In the past years, the growing threat posed by AMR and the scientific advancements unveiling its cross-sectorial nature have triggered cooperation at the global level. The World Health Assembly ratified multiple AMR-related resolutions until it adopted the Global Action Plan on Antimicrobial Resistance at the Sixty-eight WHA in 2015. This blueprint for tackling AMR globally sets out WHO’s objectives on AMR:
- improve awareness and understanding
- strengthen surveillance and research;
- reduce incidence of infection
- optimize the use; and
- develop the economic case for sustainable investment that takes account of the needs of all countries and to increase investment in new medicines, diagnostic tools, vaccines and other interventions.
WHO’s GAP on AMR stimulated action from other UN agencies, international organizations and member states.
AMR at the United Nations General Assembly
The United Nations General Assembly welcomed the GAP in resolution 70/183 on “Global health and foreign policy: strengthening the management of international health crises” at its 70th Session. The resolution requested for the organization of a high-level meeting on antimicrobial resistance in 2016, which modalities were established in res. 70/297. At the High-Level Meeting on Antimicrobial Resistance, UNGA 71st session adopted a political declaration on AMR, calling for national, regional and global work.
- To kick-start the implementation of the political declaration, then UN Secretary General Ban-Ki Moon established an ad hoc Interagency Coordination Group on Antimicrobial Resistance to guide actors and actions in the fulfillment of the GAP on AMR.
- After several meeting held between 2017 and 2019, the IACG launched its report to the Secretary General No time to Wait: Securing the future from drug-resistant infections in April 2019.
- At the 73rd session of the UNGA, Secretary General António Guterres issued its report Follow-up to the political declaration of the high-level meeting of the General Assembly on antimicrobial resistance (A/73/869) tracking progress since the political declaration.
- In April 2021, the High-Level Interactive Dialogue on Antimicrobial Resistance has been organized in the context of the 75th session of the UNGA. On the concluding day of the dialogue, the Group of Friends on AMR presented a Call to Action on AMR.
- At the 77th session of the General Assembly, the Global Leaders Group hosted a side event on AMR, urging leadership and action on Antimicrobial Resistance.
- A UNGA High-Level Meeting has been scheduled in 2024. Preparatory sessions consisted in a side-event organized by the Global Leaders Group in the context of UNGA 77th Session, in September 2022. → Political Leadership and Action on Antimicrobial Resistance: The Road to the 2024 UNGA High-level Meeting on AMR.
AMR at the United Nations Environment Assembly
UNEA-3 | Environment and health Resolution 3/4 of the Third Session of the United Nations Environment Assembly (UNEA-3), held in 2017, recognized the need to gather more understanding on the interlinkages between the environment and antimicrobial resistance. This resulted in the production of various reports and led to the UNEP adherence to the Tripartite partnership for One Health, now the Quadripartite.
UNEA-5 | Biodiversity and Health Resolution 5/6 of the Fifth Session of the United Nations Environment Assembly invites all Member States and relevant stakeholders, including the private sector, to contribute to raising awareness and understanding of the importance of addressing antimicrobial resistance,.
AMR and Agenda 2030
The challenges posed by antimicrobial resistance hinder the achievement of the Sustainable Development Goals (SDGs), as it is linked to poverty, health, food and security, and economics and work. In 2020, SGD 3.d (“strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks) was complemented with two AMR-related indicators:
- d.1 ‘International Health Regulations (IHR) capacity and health emergency preparedness’
- d.2 ‘Percentage of bloodstream infections due to selected antimicrobial-resistant organisms’
The Quadripartite Partnership
On the blueprint of the WHO’s Global Action Plan on AMR, the Food and Agriculture Organization (FAO) and the World Organization for Animal Health (WOAH, originally OIE) developed their own strategies on AMR. WHO, FAO and WOAH cooperated to address AMR under the Tripartite Partnership on One Health. UNEP collaborated with the Tripartite and joined them in 2022 in a Quadripartite collaboration addressing the risks at the human-animal-environment interface.
The Quadripartite partnership also serves as secretariat to the Global Leaders Group on Antimicrobial Resistance (GLG). The GLG was established in November 2020 following the recommendations of the IACG. It is chaired by Her Excellency Mia Amor Mottley, Prime Minister of Barbados and members include: heads of states, ministers, senior representatives of foundations and civil society organizations and private sector.
In January 2023, the Quadripartite established the Technical Group on Integrated Surveillance on Antimicrobial use and resistance to provide support on monitoring and surveillance to both the Quadripartite and the GLG.
On the sidelines of the sixth meeting of the GLG, held on 7-8 Feburary 2023 in Barbados, UNEP launched its report Bracing for Superbugs: strengthening environmental action in the One Health response to antimicrobial resistance -> Watch the press conference.
On 27 and 28 March 2023, at their first annual meeting as Quadripartite alliance for One Health, FAO, WHO, WOAH and UNEP launched a call to action for enhancing collaboration and cross-sector commitments to address global health emergencies. Priority actions all countries should undertake, include:
- Prioritize One Health in the international political agenda, increase understanding and advocate for the adoption and promotion of the enhanced intersectoral health governance;
- Strengthen national One Health policies, strategies and plans;
- Accelerate the implementation of One Health plans;
- Build intersectoral One Health workforces;
- Strengthen and sustain prevention of pandemics and health threats at source;
- Encourage and strengthen One Health scientific knowledge and evidence creation and exchange; and
- Increase investment and financing of One Health strategies and plans.
In June 2023, the Quadripartite Launched the One Health Priority Research Agenda for AMR, identifying five pillars: transmission, integrated surveillance, interventions, behavioural insights and change, and economics and policy. In addition, an equity lens with cross-cutting themes such as gender, vulnerable populations and sustainability was applied.
Other global initiatives
- The Global High-Level Ministerial Conference on Antimicrobial Resistance is a gathering of ministers, civil society, IOs, experts and the private sector from all over the world fostering collaboration to tackle AMR. It aims at accelerate political commitment. The third meeting was held in Oman from 24 to 25 November 2022. The first and second meetings took lace in 2014 and 2019 in the Netherlands. The last HLM Conference was organzied under the theme “The AMR Pandemic: From Policy to One Health Action”, paving the way to 2024 UN General Assembly High Level Meeting on AMR. Read the Muscat Ministerial Manifesto. → Read about the Quadripartite reaction here.
- The AMR Multi-Stakeholder Partnership Platform was launched in November 2022 by the Quadripartite, coordinating the action of different stakeholders active on One Health. → Learn more here and find out how to contribute by joining the fourm.
- The G20 recognized and committed to intensifying action on AMR in the Bali Declaration, following the summit held in Indonesia from 15 to 22 November 2022. Prior to that in 2017 the G20 Health Ministers issues a Berlin Declaration of the G20 Health Ministers on AMR.
- AMR Community Exchange | The WHO AMR Community Exchange is a global online collaborative space established to enable those developing, implementing and monitoring national action plans to address antimicrobial resistance (AMR) to have access to prompt advice, guidance and peer support for operational challenges. It also provides space for informal peer to peer discussions on lessons learned, challenges, enablers and innovative solutions.
National Level Action
In response to WHO 2015 Global Action Plan, 170 countries have adopted National Action Plans on Antimicrobial Resistance (NAPs AMR) and more are in the process of developing theirs. → Consult the Library of AMR national action plans
To fulfill their objectives and to align with the Global Action Plans, countries voluntarily submit their AMR-related activities and submit it on the Global Database for Tracking AMR Country Self Assessment Survey (TrACSS). → Read Switzerlands’s 2022 Country Report
In 2016 WHO, in partnership with FAO and WOAH published a manual for developing national action plans, followed in 2022 by a WHO implementation handbook. → Visit WHO dedicated webpage
In August 2023, the Quadripartite Alliance on AMR (FAO, UNEP, WHO and WOHA) published a Guidance to facilitate monitoring and evaluation for antimicrobial resistance national action plans.
One Health Approach to AMR
Considering the interconnectedness between humans, animals and the environment in the development and spread of AMR, a One Health approach is key to address AMR. The One Health High Level Expert Panel (OHHLE) – the advisory panel convened by WHO, FAO, WOHA and UNEP operational definition of One Health:
One Health is an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems. It recognizes the health of humans, domestic and wild animals, plants, and the wider environment (including ecosystems) are closely linked and inter-dependent.The approach mobilizes multiple sectors, disciplines and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems, while addressing the collective need for clean water, energy and air, safe and nutritious food, taking action on climate change, and contributing to sustainable development
The Role of Business in Countering AMR
Pharmaceutical and chemical production sectors often have lax regulations on environmental targets. Nevertheless, calls to action launched in the past years have stimulated the voluntary engagement of various pharmaceutical companies to improve the environmental footprint of the private sector and to prevent the aggravation of antimicrobial resistance. In 2016, the Davos Declaration by the Pharmaceutical, Biotechnology and Diagnostics Industries on Combating Antimicrobial Resistance, hosted by the International Federation of Pharmaceutical Manufacturers Associations (IFPMA), has been signed by more than 100 pharmaceutical, biotechnology and diagnostics companies. The Declaration inscribes their pledge to:
- Reduce the development of drug resistance;
- Increase investment in R&D that meets global public health needs:
- Improve access to high-quality antibiotics for all.
As a follow-up, thirteen major global pharmaceutical companies have launched the Industry Roadmap for Progress on Combating Antimicrobial Resistance, aligning and furthering the intentions of the Davos Declaration. → Read the text of the Industry Roadmap for Progress here.
More than 100 biotech, diagnostics, generics and research-based pharmaceutical companies and associations are now part of the AMR Industry Alliance, created in 2017 and with its secretariat based in Geneva. The Alliance is up-taking a different pharmaceutical and chemical production model, mitigating the environmental impact of manufacturing, providing guidance on the appropriate use of antibiotics and antimicrobials, and investing in research to counter the spread of AMR.
Other initiatives include the global AMR surveillance data sharing platform launched by the Center for Global Clinical Research Data Vivli, based in the USA. This platform allows companies to share data on products that are essential for research to understand and act upon the newest developments in AMR.
AMR and Standards
Surveillance and monitoring are fundamental to allow full understanding and develop adequate responses to AMR. Standards can play a crucial role in favoring a sound use of antibiotics during production, use and disposal and limiting the spread of AMR in humans, animals and in the environment. Although international standards regulating the production, use and disposal of antibiotics are not yet been established, important steps in that direction have been taken. Pursuant resolution WHA68.7 endorsed by the World Health Assembly during its Sixty-eighth session in 2015, WHO launched the Global Antimicrobial Resistance and Use Surveillance System (GLASS) in an attempt to globally standardize AMR surveillance.
In 2018 the AMR Industry Alliance established a Common Antibiotic Manufacturing Framework to set up responsible levels for both production and waste disposal. In 2022 this translated into the Antibiotic Manufacturing Standards, developed with the support of BSI Standards Limited (BSI). The standards establish a safe level at which substances will not bear adverse effects on the environment.
FAO is currently in the process of developing The International FAO Antimicrobial Resistance Monitoring (InFARM) System to support national efforts to regularly generate and analyze reliable and comparable AMR data in food and agriculture and AMU data in crops.
World Antimicrobial Awareness Week (WAAW)
The World Antimicrobial Awareness Week (WAAW) is a global campaign that is celebrated annually to improve awareness and understanding of AMR and encourage best practices among the public, One Health stakeholders and policymakers, who all play a critical role in reducing the further emergence and spread of AMR.
It place every year from 18 to 24 November since 2015, following the endorsement of a global action plan to tackle the growing problem of resistance to antibiotics and other antimicrobial medicines at the Sixty-eighth World Health Assembly in May 2015. One of the key objectives of the plan is to improve awareness and understanding of AMR through effective communication, education and training.
WAAW 2023 | Preventing antimicrobial resistance together
WAAW 2022 | Preventing Antimicrobial Resistance Together
WAAW 2021 | Spread Awareness, Stop Resistance
WAAW 2020 | Handle with care: United to preserve antimicrobials
WAAW 2019 | The future of antibiotics depends on all of us
WAAW 2018 | Change Can’t Wait. Our Time with Antibiotics is Running Out
WAAW 2017 | Seek advice from a qualified healthcare professional before taking antibiotics
WAAW 2016 | Antibiotics: Handle with Care
WAAW 2015 | Antibiotics: Handle with Care
The Role of Geneva
Organizations are listed in alphabetical order
Food and Agriculture Organization Geneva Office
The Food and Agriculture Organisation (FAO) is the United Nations specialized agency leading action to eradicate hunger and promote food sustainability. Given the importance of agriculture and animal husbandry in the development of AMR, FAO is a frontrunner in tackling this challenge. Following its 39th Conference in 2015, FAO passed Resolution 4/2015 on the threat of antimicrobial resistance. Consequently, it launched its first Action Plan on Antimicrobial Resistance in 2016 and renewed its strategy again in 2021. The Action plans of address four major focus areas:
- awareness and engagement;
- surveillance and monitoring;
- strengthened governance;
- promotion of good practices and of responsible use of antimicrobials
FAO is part of the Quadripartite Partnership on AMR together with WHO, WOAH and UNEP. FAO also collaborates with WHO to monitor the health impacts of pesticides residues in food through the Joint FAO/WHO Meeting on Pesticide Residues (JMPR). This independent body of scientists establishes the limits for safe intake of pesticides through eating food during a life time based on the assessments of data of national registrations of pesticides worldwide and scientific studies.
At the beginning of 2022, FAO also began the development of The International FAO Antimicrobial Resistance Monitoring (InFARM) System, supporting nations in the effort of producing reliable and comparable AMR data in food and agriculture and AMU data in crops.
Global Antibiotic Research & Development Partnership
Global Antibiotic Research & Development Partnership (GARDP) was created in 2016 by the WHO and the Drugs for Neglected Disease initiative (DNDi). GARDP is a frontrunning initiative collaborating with public and private sectors to preserve the effectiveness of antibiotics, accelerating its development and facilitating access.
Rosa-Luxemburg-Stiftung Geneva Office
The Rosa-Luxemburg-Stiftung Geneva Office addresses various topics related to health as part of it mandate to foster socio-ecological transformation and to the implementation of social rights on a global scale. This includes publications, among which ‘Untangling antimicrobial resistance (AMR)‘, published in October 2022.
South Center
The South Centre is an intergovernmental policy research think-tank composed of and accountable to developing country Member States. It conducts policy-oriented research on key policy development issues, and supports developing countries to effectively participate in international negotiating processes that are relevant to the achievement of SDGs. The Centre promotes the unity of the South in such processes while recognizing the diversity of national interests and priorities. The South Centre is committed to support the efforts of Civil society organizations (CSOs) based in developing countries in the design and launch of campaigns in the lead to the annual World Antimicrobial Awareness Week (WAAW).
United Nations Environment Programme (UNEP) Chemicals and Health Branch
The Chemicals and Health Branch leads global action on the environmentally sound management of chemicals and waste. Antimicrobial resistance among the emerging issues of environmental importance, advocating for coordinated action to address AMR challenges and the triple planetary crisis.
World Bank Group Geneva Office
The World Bank Group addresses antimicrobial resistance through economical and technical analysis and by financing projects to improve WASH conditions. The World Bank also collaborates with international organizations and countries to imrpove awareness, as well as organizing events and producing reports.
World Economic Forum
The World Economic Forum dedicates publications and articles to cross-cutting issues of antimicrobial resistance, from agriculture and livestock, to water, to economic and health risks. Among these, a briefing paper in collaboration with the Swiss Agency for Development and Cooperation addressed AMR in water.
World Health Organization
The World Health Organization is on the frontrun of addressing antimicrobial resistance. In 2016 WHO adopted a Global Action Plan on Antimicrobial Resistance (GAP) to counter one of the major threats to effective global public health. The GAP is set to achieve five interrelated goals:
- to improve awareness and understanding of antimicrobial resistance through effective communication, education and training;
- to strengthen the knowledge and evidence base through surveillance and research;
- to reduce the incidence of infection through effective sanitation, hygiene and infection prevention measures;
- to optimize the use of antimicrobial medicines in human and animal health; and
- to develop the economic case for sustainable investment that takes account of the needs of all countries and to increase investment in new medicines, diagnostic tools, vaccines and other interventions.
Various bodies within WHO are active on AMR, coordinated by the Department of Global Coordination and Partnership on Antimicrobial Resistance for the One Health approach and by the Surveillance, Prevention and Control Department on technical matters. WHO action on AMR is supported by the Strategic and Technical Advisory Group for Antimicrobial resistance (STAG-AMR). → To stay updated on the most recent WHO’s activities and findings related to Antimicrobial Resistance, sign up to the WHO Antimicrobial Resistance Division Quarterly Newsletter
World Organization for Animal Health
The World Organization for Animal Health (WOAH, founded as OIE) is global authority on animal health. WOAH cooperates with national-level Veterinary and Aquatic Animal Health Services, collects and analyzes data on antimicrobial use in animals, and carries out advocacy activities. Most importantly, WOAH plays a key role in setting international standards with regards to prudent and responsible use of antimicrobial agents. On top of that, since 2015 WOAH compiles global and regional trends of on Antimicrobial Agents Intended for Use in Animals into an annual report. → Read the Sixth Annual Report on Antimicrobial Agents Intended for Use in Animals (WOAH, 2022)
On the model of WHO Global Action plan, WOAH developed in 2016 its Strategy on Antimicrobial Resistance and the Prudent Use of Antimicrobials, joining forces with WHO, FAO and UNEP in the Quadripartite partnership. The goals of WOAH in tackling AMR are:
- Improve awareness and understanding
- Strengthen knowledge through surveillance and research
- Support good governance and capacity building
- Encourage implementation of international standards
World Trade Organization
Surveillance and monitoring of antimicrobials and antibiotics throughout their life cycle have important trade implications. The WTO Agreement on Sanitary and Phytosanitary Measures (SPS Agreement) and Agreement on Technical Barriers to Trade (TBT Agreement) can provide a legal basis for potential international standards for antibiotics production, use and access. WTO has collaborated with WHO and the Wolrd Intellectual Property Organization (WIPO) on publications on Intersections between public health, intellectual property and trade (WHO, WIPO, WTO | 2020) and events.
Local Geneva & Switzerland
Republic and State of Geneva
The Cantonal Health Authority ( direction générale de la santé – DGSA collects and diffuses information on the risks related to antimicrobial resistance and takes part in local and international initiatives to counter such threats. For instance, on the occasion of World Antibiotic Awareness Week 2023, it developed a game to help people better understand the issues surrounding antibiotic resistance.
Federal Office of Public Health
The Swiss Federal Office of Public Health (FOPH) is active on circulating information and rasing awareness on antimicrobial resistance. In 2015, it published the National Strategy on Antimicrobial Resistance (StAR) to ensure the continued effectiveness of antimicrobials. In collaboration with the Federal Food Safety and Veterinary Office, and the Federal Office for the Environment, FOPH recently published the “Swiss Antibiotic Resistance Report 2022”, which showcased positive trends of decreasing numbers of prescribed antibiotics in the country, suggesting the effectiveness of the Strategy on Antibiotic Resistance,.
The Swiss Federal Office of Public Health together with the Institute for Infectious Diseases (IFIK) of the University of Bern is a supporter of the ANRESIS, the Swiss Centre for Antibiotic Resistance, which monitors the development of antibiotic resistance in Switzerland since 2014.
Swiss National Science Foundation
The Swiss National Science Foundation launched in 2016 a National Research Project on Antimicrobial Resistance (NRP 72) aiming to preserve antibiotics effectiveness. Forstering collaboration between science and medicine, the project implements the One Health approach.
Academic Institutions
Global Health Center of the Geneva Graduate Institute
The Global Health Center of the Geneva Graduate Institute addressed the topic of AMR in events, publications and policy briefs.
University of Geneva
The University of Geneva established a focus group on the topic “Epidémiologie et contrôle de la résistance aux antibiotiques” conducting studies and publishing articles on the topic.
Learning
- Antimicrobial Resistance Course Series | WHO
- FAO Antimicrobial Resistance video playlist | FAO
- ReAct Toolbox for Action on Antibiotics Resistance
- Navigating the Tripartite Zoonoses Guide (TZG): A training for advocates and implementers | FAO, OIE, WHO
- 6 steps for sustainable implementation of national action plans on antimicrobial resistance | WHO



